A European consortium coordinated by CNCR investigator Ruud Toonen receives 1 million euros for epilepsy research.
Epilepsy is a severe and disabling disease affecting about 1% of the world’s population. Despite years of intense research about 30% of all epilepsies cannot be treated by available drugs. To develop new and better treatment options, a detailed knowledge of the mechanisms leading to epilepsy is urgently required. Toonen will lead the ERA-NET NEURON transnational research project “SNAREopathy” that will focus on a group of difficult-to-treat, severe epilepsies caused by mutations in genes that mediate the communication between nerve cells (synaptic transmission). The consortium unites experts in the genetics of epilepsy and neurobiologists working on synaptic transmission from the Netherlands, Germany, Italy and Norway to identify the mechanisms leading to epilepsy using several sophisticated mouse and zebrafish models, as well as human cell models derived from skin biopsies that will be transformed into human neurons (so-called iPSC-derived neurons). Based on the identified epileptic mechanisms, the consortium will use these models for drug screening to search for novel medications to better and more specifically treat the severely affected epilepsy patients.

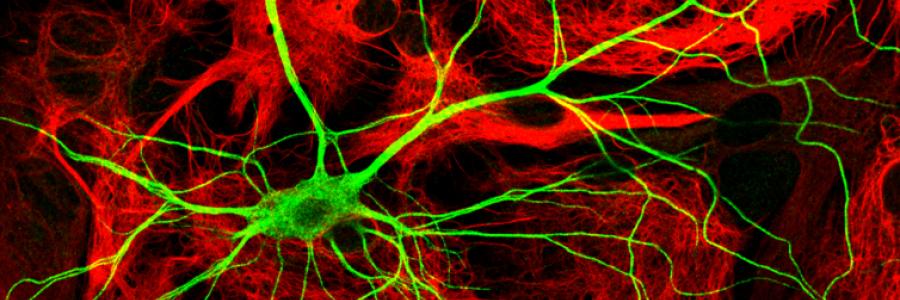
The interaction of SNAREs (soluble N-ethylmaleimide–sensitive factor-attachment protein receptors) and STXBP1/MUNC18-1, together with calcium binding proteins of the synaptotagmin family ensures the speed and precision of neurotransmitter release. Importantly, mutations in two central components of the SNARE-complex and one co-factor, encoded by the STX1B, STXBP1 and PRRT2 genes (See Figure), lead to a wide spectrum of seizure phenotypes and other neuropsychiatric symptoms, many of which respond poorly to available antiepileptic drugs. Interestingly, the same genes are associated with autism and schizophrenia disorders with an increased seizure comorbidity. We have identified mutations in two of the three genes, STX1B & PRRT2, in familial or sporadic forms of epilepsy. Similar to but clinically distinguishable from STX1B mutations, de novo mutations in STXBP1 cause a severe, early onset epilepsy with a characteristic suppression-burst pattern in the EEG. We will now combine our knowledge of these presynaptic proteins to reach a comprehensive picture of presynaptic dysfunction in epileptic disorders and related comorbidities using animal models, patient-derived neurons and innovative in vitro and in vivo screening platforms to develop new tailored therapeutic approaches.